The metabolic syndrome: What’s in the name?
There is currently no consensus definition of the metabolic syndrome, although the clustering of metabolic abnormalities, such as central obesity, impaired glucose tolerance and type 2 diabetes, dyslipidemia and hypertension has been noted in certain patients for many years. Recently more components of the syndrome have been proposed, including vascular inflammation, hypercoagulability, hyperuricemia and microalbuminuria. According to Reaven (1) it is necessary to make a distinction between metabolic syndrome as a diagnostic category and metabolic syndrome as a pathophysiologic entity designating a cluster of related metabolic abnormalities. Studies over the last 25 years have provided the evidence that insulin resistance at the level of muscle and adipose tissue was the common abnormality that increased the likelihood of an individual developing, not only type 2 diabetes, but also cardiovascular disease (2). The concept of the metabolic syndrome viewed as precursor to the development of both type 2 diabetes and cardiovascular disease has progressively emerged with a formal recognition by the World Health Organization (WHO) in 1998 and the National Cholesterol Education Program Adult Treatment Panel III in 2001 (NCEP ATP III), which has recently proposed a formal definition of the metabolic syndrome.
The syndrome is a multi-component disease brought on by combination of lifestyle and environmental factors, with some populations exhibiting a genetic susceptibility for its development. Over years several reports have been published indicating that the common ingredient has been insulin resistance, and it has been speculated that it may be mediated in part by an increase in FFA accompanied by an overproduction of triglyceride-enriched particles and increased small dense LDL particles.
In the prospective Cardiovascular Munster study (PRO-CAM), 4559 male participants were examined for cardiovascular risk factors and kept under observation to record mortality and cardiovascular events including myocardial infarction and stroke. Interestingly, the results showed that a high triglyceride level in absence of high LDL/low HDL does not increase the risk of CHD.
However if the LDL/HDL ratio is higher than 5, then an increased triglyceride level confers an additional risk (6). The importance of the triad of high triglycerides, low HDL and elevated LDL cholesterol has been further supported by recent analysis of the Helsinki Heart Study (7). Taken together, the above data suggest that hypertriglyceridemia/low HDL cholesterol syndrome constitutes a powerful risk factor for non-fatal myocardial infarction or coronary artery disease death that would escape attention if LDL levels alone were determined. For practical purposes, it appears advisable to base risk prediction of atherosclerotic coronary artery disease and treatment decision on a full lipid profile rather than cholesterol alone or LDL-cholesterol determination.
In order to understand the role of hyperlipemia in the development of CHD, it is important to examine what happens at the endothelial level. LDL-cholesterol passes across the endothelium and is modified by stimulating macrophage chemoattractant protein-1 (MCP-1) to recruit monocytes, and also by stimulating differentiation in macrophages which express scavenger receptors that take up lipid to make foam cells. The foam cells produce growth factors and proteinases and they also release cytokines to stimulate adhesion proteins. HDL has multiple effects and can block the atherogenic process at several levels. The best known is the efflux of cholesterol from foam cells and the prevention of foam cell formation. HDL also prevents the oxidizing modification of LDL within the intima. HDL has been shown to inhibit the cytokine-induced expression of adhesion proteins and to inhibit MCP-1. It is also anti-thrombotic and anti-apoptotic. It has been generally accepted that 1% increase in concentration of HDL-cholesterol predicts a 1% reduction in coronary events, independent of the changes in LDL-cholesterol.
Nofer has demonstrated that HDL exerts many anti-inflammatory effects, as illustrated in experimental models of atherosclerosis and in true models of inflammation. ApoA-I and lysosphingolipids can account for many of the anti-inflammatory effects of HDL.
Oxidized low-density lipoprotein cholesterol (ox-LDL) may increase cytokine expression (IL-1ß, TNF-α; IL-6 and IL-8) in endothelial cells. This event is followed by vascular cell adhesion molecules, VCAM-1 and ICAM-1. Isolated HDL and reconstituted HDL inhibit the expression of these cytokines in isolated endothelium cells. Further studies are underway to clarify the influence of HDL on the expression of endothelial cell adhesion molecules.
Insulin resistance and lipid disorders
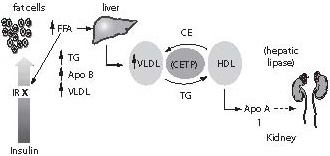
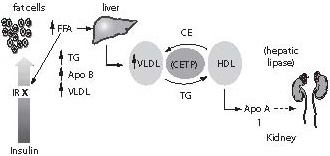
Among several causes of insulin resistance, it has been speculated that it may be mediated in part by an increase in free fatty acids (FFA) that inhibits post-insulin receptor signalling and thus contributes to insulin resistance. FFA may also be an important determinant of the metabolic syndrome as their level is generally high in this condition (Figure 1). As resistance to insulin action or insulin deprivation is associated with increased lipolysis, intra-abdominal fat, which is metabolically very active, releases FFA into portal circulation. The liver converts FFA into triglycerides and this may explain the relationship of hypertriglyceridemia and the metabolic syndrome. Increased supply of glucose and overproduction of VLDL raises the concentration of triglyceride-enriched particles, leading to a reciprocal exchange of fatty acids: cholesterol-esters are transferred to VLDL and chylomicron remnants, while triglycerides are transferred to LDL and HDL particles to form small-dense LDL and HDL. These dense particles are well known for their high atherogenic potential.
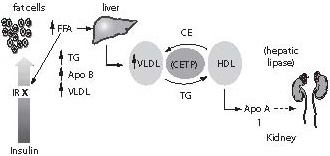
Figure 1. Mechanisms relating to insulin resistance and dyslipidemia
Besides available pharmacological remedies used to decrease insulin resistance, exercise and weight loss represent the key steps as they are widely implemental and rather inexpensive. Exercising increases GLUT-4 receptors in skeletal muscles using glucose with a reduction in insulin resistance.
Several growth factors and cytokines can modulate insulin post-receptor signaling. While IGF-1 enhance insulin action mediated by its cellular receptor, FFA, TNF-α (a pro-inflammatory cytokine mainly produced by activated macrophages), and leptin seem to have the opposite effect (8). TNF-α impairs insulin signaling by serine phosphorylation of IRS-1 and inhibits insulin receptor tyrosine kinase activity, which leads to impaired downstream signaling (5). As TNF-α plasma concentration is increased in obesity, sepsis and cancer, this may in part explain why patients presenting with these conditions often exhibit abnormal glucose metabolism. The action of leptin on glucose disposal seems to be more equivocal in increasing phosphorylation of IRS-1 and IRS-2; on the other hand, leptin seems to be associated with insulin resistance as a strong correlation has been found between plasma leptin levels and insulin resistance in obese people, inhibiting post-receptor insulin signaling and action.
Lipid risk factors
One of the major risk factors in metabolic syndrome is dyslipidemia which can be related to a changed lipoprotein spectrum and to modified lipoproteins.
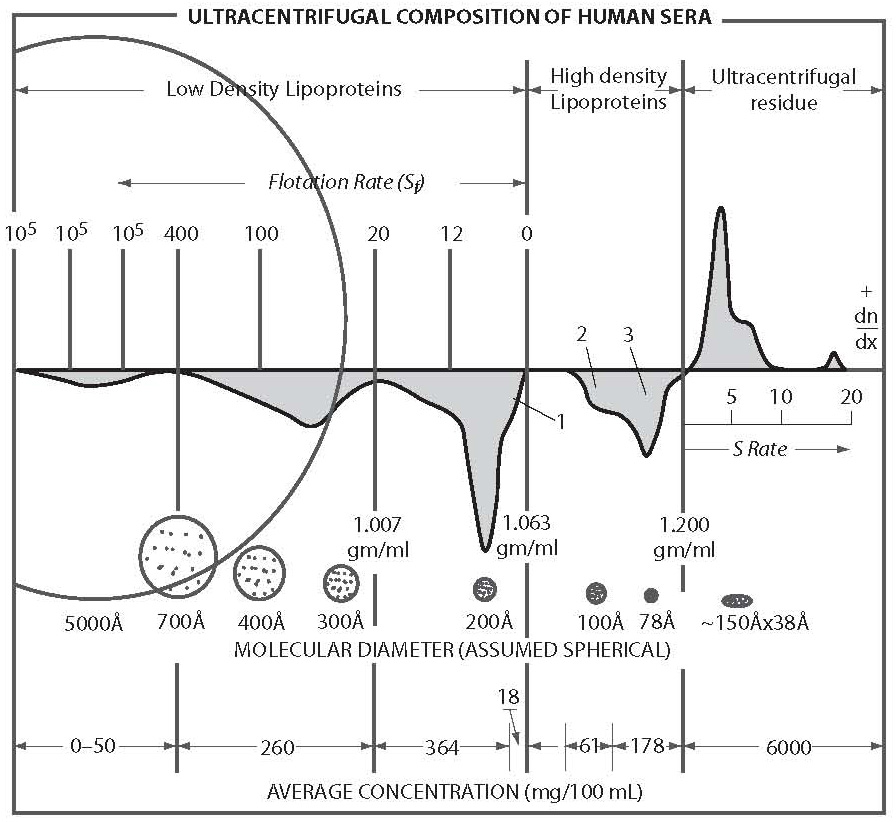
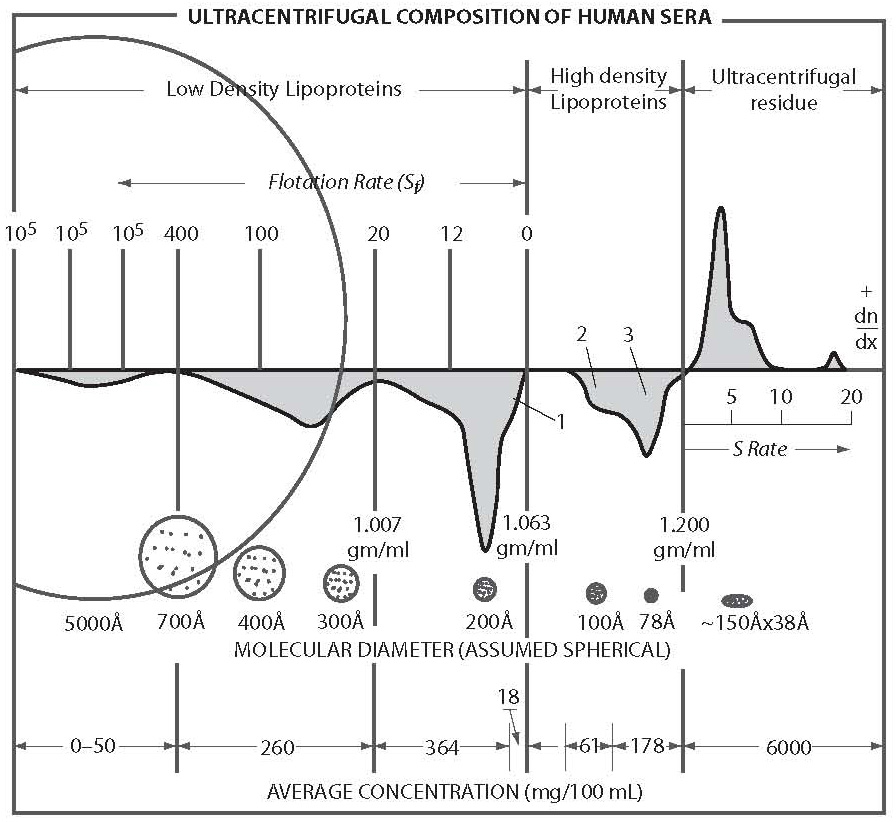
A first step in separation and identification of serum lipoprotein classes was ultracentrifugation. Goffman and Lindgren were the first to separate serum lipoproteins in different density classes based on density gradients (Figure 2).
Figure 2. Ultracentrifugation image of plasma lipoproteins, Characterized in size (Å), density range (g/mL), concentration (mg/100 mL) and flotation rate (Sf).
They were able to characterize particle sizes and relate them to the risk in coronary heart events. We have had to wait till now to understand more about the relationship between physical parameters of molecules and the risk for disease. It is a challenge for the future to explore the influence of physical parameters of a particle on the development of a disease, to find methods for diagnostic possibilities and also to explore the ways of treatment.
Ultracentrifugation performed by Gofman and Lindgren in the 1950s (i.e. in 1952) and introduced by Svedberg became the reference method for lipoprotein separation and is still the golden standard for lipoprotein separation, identification and classification. They are characterized by the size of particles (Å), density range (gm/mL), flotation rate (Sf) and concentrations (mg/mL). Since the introduction of this method, we have known that LDL lipoproteins are present in most cardiovascular events and that HDLs are considered protective against CVD.
Total cholesterol does not accurately predict the risk of CVD, the decision on treatment is based on LDL-cholesterol, but LDL heterogeneity may also be taken into account. Small dense LDL particles are more atherogenic than large, buoyant LDL particles, and ox-LDL also increases atherogenicity. Particle dimensions are very soon to become a diagnostic tool. Gradient gel electrophoresis without the use of denaturing conditions is commonly applied to characterize particle size distribution. High-performance gel-filtration chromatography and nuclear magnetic resonance (NMR) spectroscopy have been recently applied for determinations of LDL particle size. Different methods of density gradient ultracentrifugation have been used to characterize LDL flotation rates, and several methods have been employed on discontinuous salt gradients to determine LDL subclasses based on density. Various methods of determining LDL subclasses show a high degree of correlation despite the fact that they measure different physical properties of LDL.
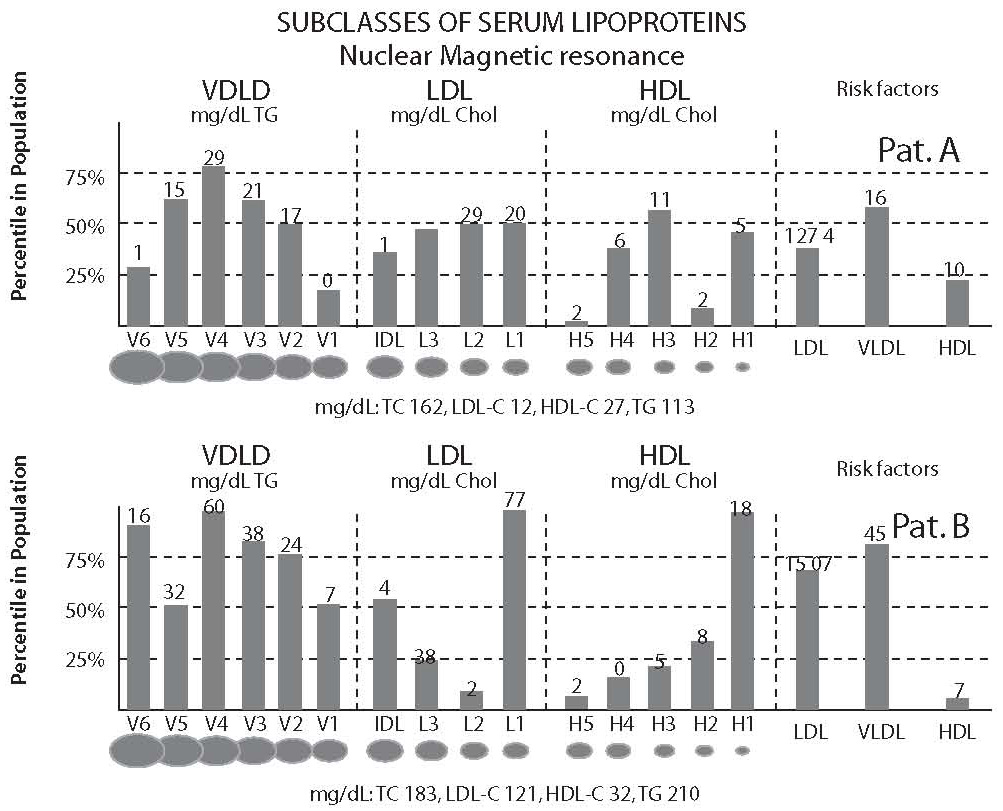
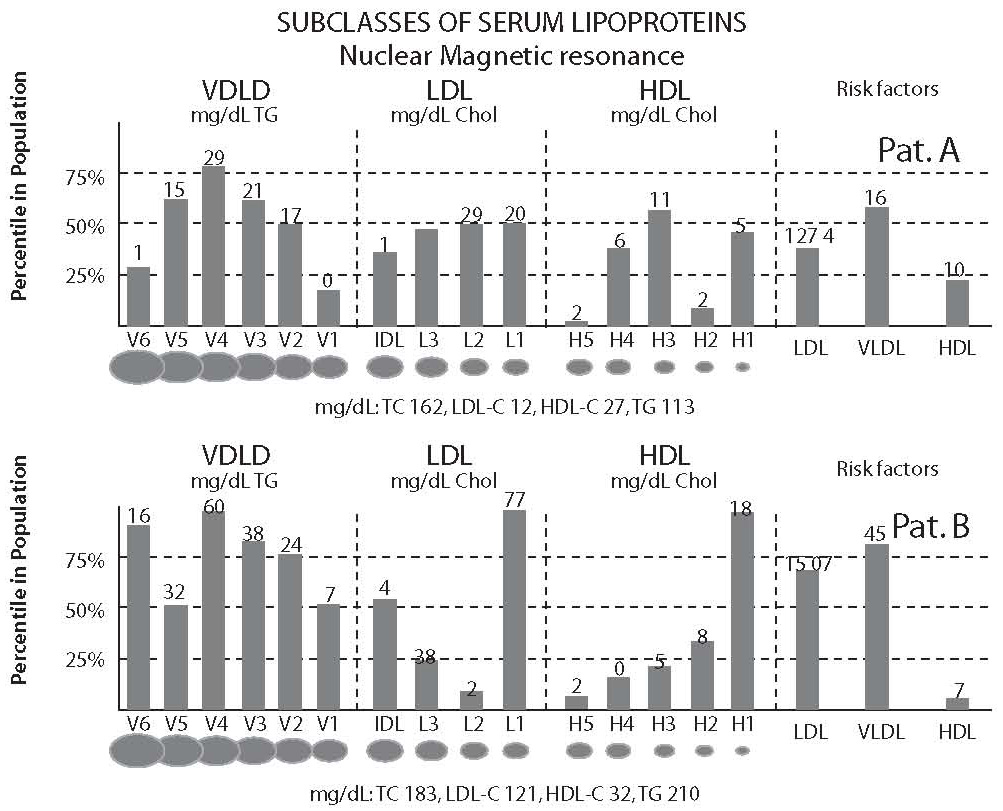
The new procedure exploits what appears to be natural but has generally been unappreciated, i.e. proton NMR spectroscopic differences exhibited by lipoprotein particles of different sizes. The new process has now largely been complete. Using a dedicated intermediate-field (360 MHZ) NMR analyzer, routine quantification of 15 different subclasses of VLDL, LDL and HDL has been achieved in about one minute. In the European Prospective Investigation into Cancer and Nutrition (EPIC Study) (9), the relationship between LDL particle number and sizes were studied by NMR, together with LDL-cholesterol concentration and the risk of future coronary artery disease. LDL particle number was related to CAD also after adjustment for LDL-cholesterol concentration. In figure 3, NMR profiles of lipoprotein distribution of two middle-aged patients (A and B) illustrate how different the underlying metabolic status and associated risk of CHD can be for two people who have virtually identical LDL and HDL cholesterol levels with, however, differences in CVD risk (Figure 3).
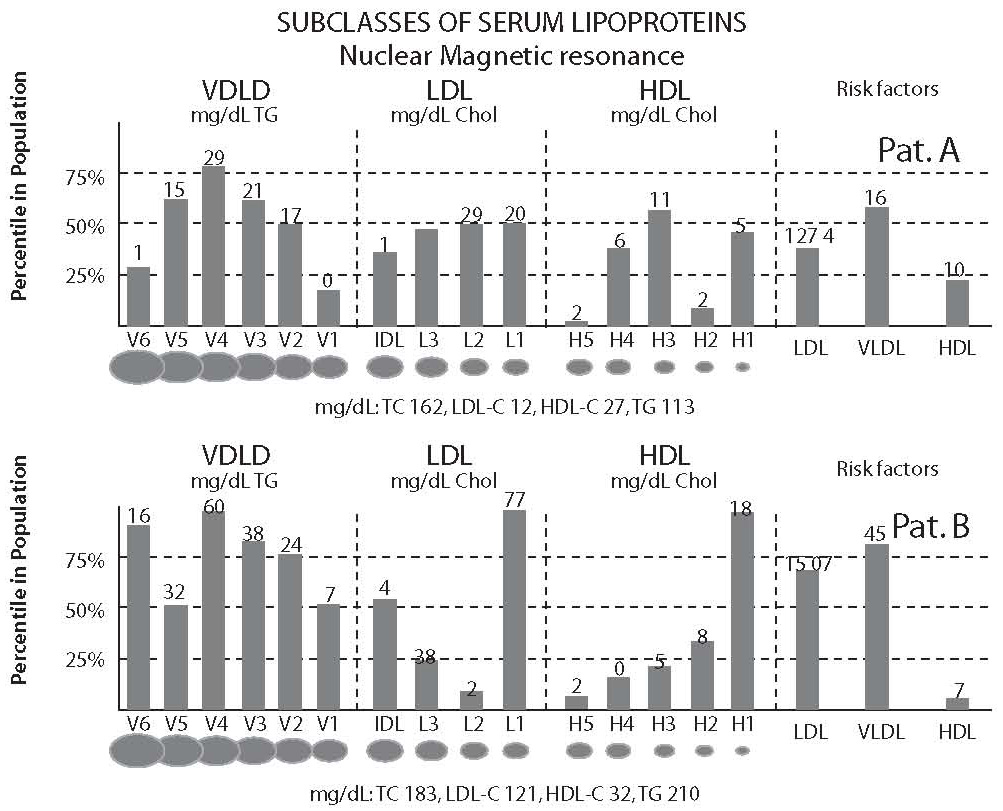
Figure 3. NMR profiles of lipoprotein distribution of patients A and B
Nuclear magnetic resonance spectroscopy measures the plasma concentration of lipids in most lipoproteins, and it can be used to estimate particle concentration. The technique also measures the size of the lipoprotein particle. In a cohort of middle-aged women in Women’s Health study, high significance between cardiovascular events and particle numbers has been shown also after adjusted cholesterol/HDL and triglycerides; however, the particle size alone was not determined to be a contributor to risk events. Nevertheless, there is a direct relation between the size of the LDL particle and the rate of ox-LDL (10).
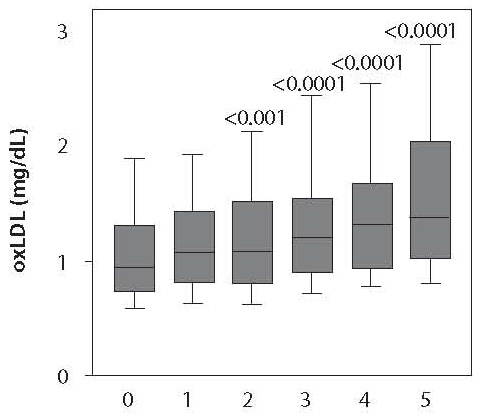
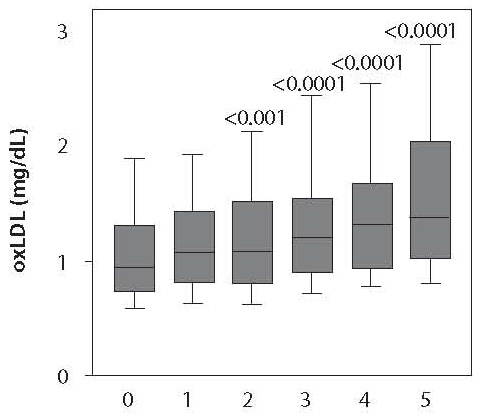
Small LDL particles are more susceptible to oxidation and ox-LDL is an independent risk factor for CVD. The relationship between ox-LDL and different components of metabolic syndrome has been examined in a population study of 3.030 normal functioning individuals between 30 and 75 years of age. Also, the severity of individual components was evaluated (11).
Ox-LDL was measured against ODS ratio of cardiovascular disease. The ox-LDL levels increased not only in function of the number of metabolic syndrome components but also in function of the severity of individual components (Figure 4). Monoclonal antibody mAB-4E6 formed against a neo-epitope in the aldehyde substituted by apo-B 100 in mice is used in the ELISA competition for determination of circulating ox-LDL. As a conclusion, ox-LDL can be used as a marker for the analysis of cardiovascular risk in metabolic syndrome (11).
Figure 4. Ox-LDL in function of the metabolic syndrome components. 0 = control group of subjects; 1 = subjects with one component of the metabolic syndrome (e.g. high LDL-cholesterol); 2 = subjects with two components of the metabolic syndrome (e.g. high LDL-cholesterol and hypertension); 3 = subjects with three components of the metabolic syndrome (e.g. high LDL-cholesterol, hypertension and diabetes mellitus) etc.
Metabolic syndrome: the role and importance of lipid components
Recent evidence has shown that the presence of metabolic syndrome is associated with an increased risk of coronary heart disease (CHD), myocardial infarction, and stroke in both sexes.This substantially increased risk of CV morbidity and mortality associated with the presence of metabolic syndrome appears independent of other significant, potentially confounding factors such as smoking, plasma LDL cholesterol levels or alcohol consumption.Dyslipidemia is an integral part of metabolic syndrome since both definitions include hypertriglyceridemia (defined as serum triglycerides ≥ 150 mg/dL) and a low HDL cholesterol concentration (defined as HDL-cholesterol < 40 mg/dL for men and < 50 mg/dL for women by NCEP ATP III, or HDL-cholesterol < 35 mg/dL for men and < 40 mg/dL for women by WHO) as components. Individuals with metabolic syndrome, particularly those with abdominal obesity, exhibit a highly atherogenic lipid profile which may account for their high risk of CVD. Central fat accumulation and the presence of insulin resistance have both been associated with a cluster of dyslipidemic features, i.e., elevated plasma triglyceride level, an increase in very-low-density lipoprotein (VLDL) and intermediate-density lipoprotein (IDL), the presence of small dense LDL particles, and a decrease in HDL-cholesterol. These abnormalities of lipoprotein metabolism are more likely to occur together than separately and constitute the key component traits of the metabolic syndrome.
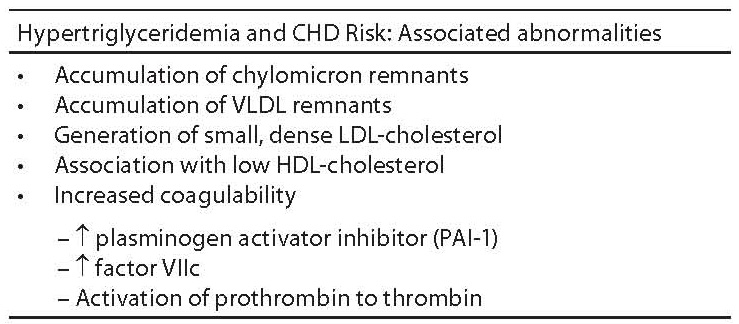
Recent prospective studies indicate that elevated triglycerides are an independent risk factor in CHD. Hypertriglyceridemia is associated with several atherogenic factors including increased concentrations of triglyceride-enriched lipoproteins and the atherogenic lipoprotein phenotype consisting of small dense LDL particles and low high-density lipoprotein (HDL) cholesterol. The factors contributing to hypertriglyceridemia in general population include obesity, overweight, physical inactivity, excess alcohol intake, high-carbohydrate diet, type 2 diabetes, and some other diseases (e.g. chronic renal failure, nephrotic syndrome), certain drugs (e.g. corticosteroids, estrogens, retinoids, high doses of adrenergic blocking agents), and genetic disorders (familial combined hyperlipidemia, familial hypertriglyceridemia, and familial dysbetalipoproteinemia). In daily practice, elevated serum triglycerides are predominantly observed in persons with metabolic syndrome. Many previous studies have indicated that hypertriglyceridaemia is strongly associated with all metabolic syndrome components. Patients with metabolic syndrome who have hypertriglyceridemia most often exhibit elevated level of triglyceride-enriched lipoproteins which are considered atherogenic. Actually, those are partially degraded VLDL, commonly called “remnant lipoproteins”. In clinical practice, VLDL cholesterol is the most readily available measure of atherogenic remnant lipoproteins. Thus, VLDL cholesterol can be a target of cholesterol-lowering therapy. Recent guidelines have identified the sum of LDL + IDL + VLDL cholesterol (termed “non-HDL cholesterol” [total cholesterol minus HDL cholesterol]) as a secondary target of therapy in persons with hypertriglyceridaemia (Table 1).
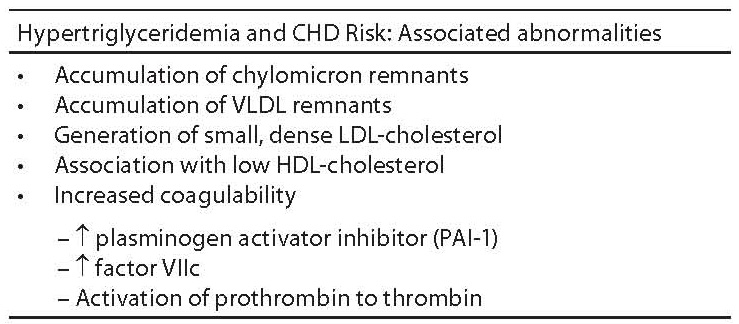
Table 1. Abnormalities associated with hypertriglyceridemia in metabolic syndrome.
Low HDL-cholesterol
Low levels of HDL-cholesterol are associated with increased risk of coronary artery disease (CAD). This relationship has been observed irrespective of age, blood pressure level, obesity, total cholesterol or LDL-cholesterol levels. The term “isolated low HDL” has been used to describe the situation where total cholesterol or LDL-cholesterol are considered normal but HDL-cholesterol is low. Long-term follow-up of subjects with low HDL-cholesterol has demonstrated that their risk of developing CAD is similar to the risk in subjects with elevated total cholesterol or LDL-cholesterol. Low HDL-cholesterol is the strongest predictor of subsequent cardiovascular events in patients with angiographically confirmed CAD and the levels of total cholesterol within normal range. According to current guidelines, the presence of low HDL-cholesterol should be considered a major cardiovascular risk factor which modifies the goal for LDL-lowering therapy and is used as a risk factor to estimate the 10-year risk for CHD. A low HDL-cholesterol level has several causes, some of which are associated with insulin resistance, i.e. elevated triglycerides, overweight and obesity, physical inactivity, and type 2 diabetes. The combination of a low HDL-cholesterol with elevated plasma triglyceride level has therefore been considered an insulin-resistant state. It should be noted that certain drugs also reduce the level of HDL-cholesterol (e.g. beta-blockers, anabolic steroids, progestational agents). Nevertheless, low HDL-cholesterol is an important component trait of metabolic syndrome and deserves close clinical attention and management since patients with this trait are at a high risk for CVD. The total cholesterol/HDL-cholesterol ratio is a well known predictor of CHD risk. We have recently shown that the men characterized by the hypertriglyceridemic waist phenotype had a substantially elevated total cholesterol/HDL-cholesterol ratio compared with those without this phenotype. In this study, only 3% of men with waist circumference < 90 cm and triglyceride levels < 2.0 mmol/L had a total cholesterol/HDL-cholesterol ratio of 6 or higher. However, almost 50% of subjects characterized by the hypertriglyceridemic waist phenotype had a ratio above 6. Similar conclusions have been reached in other study populations. The number and size of the HDL particles also play important roles in the risks of cardiovascular events in metabolic syndrome. HDL molecules have demonstrated the most important role in the dyslipidemia, yet there are many unanswered questions: what regulates HDL concentration, subpopulations and functions? The cardioprotective function of HDL and the function of HDL concentration is unknown. What is the relative contribution of cholesterol efflux, of antioxidant properties and the role of the anti-inflammatory characteristics of HDL subtypes? Further, there is no data to explain the relationship between overweight and smoking and low HDL.
Conclusion
Metabolic syndrome represents a clustering of cardiovascular risk factors linked through their association with insulin resistance (12). Since insulin resistance is an independent risk factor for cardiovascular disease, its presence can lead to macrovascular complications long before other features of metabolic syndrome are evident.
It is very important to recognize that high LDL or high total cholesterol are not components of the metabolic syndrome. In fact, LDL is often below average in patients with the metabolic syndrome. Thus, physicians must be aware that patients can still have a high risk of cardiovascular disease even if they have low LDL or total cholesterol. In essence, one can conceptualize metabolic syndrome as a “non-LDL” type of risk, and just as important as LDL to recognise and to treat. The incidence of metabolic syndrome has been increasing throughout Europe and North America, in parallel with an increase in overweight, obesity, and diabetes (13). Since LDL has been emphasised in treatment guidelines quite effectively, it is now time to turn the attention of clinicians to metabolic syndrome. If this epidemic of overweight and diabetes is not stopped, cardiovascular disease will increase and we will waste the progress we have made in the past 20 years. Metabolic syndrome requires a multi-factorial approach to treatment since all of its components combine to increase the risk of cardiovascular disease. Firstly, diet and exercise will improve all components by lowering triglycerides, glucose and blood pressure, and raising HDL. In fact, much of the metabolic syndrome can be attributed to “over nutrition”. Secondly, pharmacological therapy for improving the components of metabolic syndrome should be individualized in each patient. Challenges remaining in the identification of high-risk persons include the introduction of clinical markers of insulin resistance, integration of post challenge glucose and lipid concentrations, and better definition of the role of inflammatory, prothrombotic, and genetic factors (14). Improved understanding of the risk factors for metabolic syndrome is required, and clinical trials of therapeutic interventions specifically targeted to this syndrome need to be conducted.
Notes
Potential conflict of interest
None declared
References
1. Reaven GM. The metabolic syndrome: What is in a name? Clin Chem 2006;52:5.
2. Reaven GM. The metabolic syndrome or the insuline resistance syndrome? Different names, different concepts, and different goals. Endorcinal Metab Clin N Am 2004;33;283-303.
3. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143-421.
4. Despreés JP, Lemieux I, Prud’homme D. Treatment of obesity: need to focus on high risk abdominally obese patients. BMJ 2001;322:716-20.
5. Lamarche B, Tchernof A, Maurieége P, Cantin B, Dagenais GR, Lupien PJ, Despres JP. Fasting insulin and apolipoprotein B levels and low-density lipoprotein particle size as risk factors for ischemic heart disease. JAMA 1998;279:1955-61.
6. Assmann G, Schulte H. Relation of high density lipoprotein cholesterol and triglycerides to incidence of atherosclerotic coronary artery disease (the PROCAM experience) Am J Cardiol. 1992:70,733-7.
7. Mannienen V, Tekanen L, Koskinen P, Huttunen JK, Mänttäri M, Heinonen OP, Frick MH. Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study. Implications for treatment. Circulation 1992;85:37-45
8. Donahue RP, Prineas RJ, Donahue RD, Zimmet P, Bean JA, De Courten M, et al. Is fasting leptin associated with insulin resistance among nondiabetic individuals? Diabetes Care 1999;22:1092-6.
9. El Harchaoul K, van der Steeg WA, Stroes J, Kastelein J. Value of low-density lipoprotein particle number and size as predictors of coronary artery disease in apparently healthy men and women: the EPIC-Norfolk Prospective population study. J Am Coll Cardiol 2007;49(5):547-53.
10. Sacks FM. The apolipoprotein story. Atherosclerosis Supplements 2006;7:23-7.
11. Blaton V. Ox-LDL in function of metabolic syndrome components. Belgian Lipid Club 2005;6:4-5.
12. Haffner S. Diabetes and the metabolic syndrome - When is it best to intervene to prevent. Atherosclerosis supplements 2006;7:3-10.
13. Hu FB, Stampfer MJ, Haffner MJ. Elevated risk of cardiovascular disease prior to clinical diagnosis of type 2 diabetes. Diabtes Care 2002;25:1129-34.
14. Alexander CM, Haffner SM. NCEP defined metabolic syndrome, diabetes and prevalence of coronary heart disease. Diabetes 2003; 52(5); 1210-4.