References
1. Roth J, Zuber C, Park S, Jang I, Lee Y, Kysela KG, et al. Protein N-glycosylation, protein folding, and protein quality control. Mol Cells 2010;30:497-506.
2. Moran AP, Gupta A, Joshi L. Sweet-talk: role of host glycosylation in bacterial pathogenesis of the gastrointestinal tract. Gut 2011;60:1412-25.
3. Larkin A, Imperiali B. The expanding horizons of asparagine-linked glycosylation. Biochemistry 2011;50:4411-26.
4. Schwarz F, Aebi M. Mechanisms and principles of N-linked protein glycosylation. Curr Opin Struct Biol 2011;21:576-82.
5. Jaeken J, Vanderschueren-Lodewyckx M, Snoeck L, Corbeel L, Wggermont E, Eeckels R. Familiar psychomotor retardation with markedly fluctuating serum prolactin, FSH and GH levels, partial TBG deficiency, increased serum arylsulphatase A and increased CSF protein: a new syndrome? Pediar Res 1980;14:179.
6. Jaeken J. Congenital disorders of glycosylation (CDG): it’s (nearly) all in it! J Inherit Metab Dis 2011;34:853-8.
7. Aebi M, Helenius A, Schenk B, Barone R, Fiumara A, Berger EG, et al. Carbohydrate-deficient glycoprotein syndromes become congenital disorders of glycosylation: an updated nomenclature for CDG. First International Workshop on CDGS. Glycoconj J 1999;16:669-71.
8. Jaeken J, Hennet T, Matthijs G, Freeze HH. CDG nomenclature: time for a change! Biochim Biophys Acta 2009;1792:825-6.
9. Eklund EA, Freeze HH. The congenital disorders of glycosylation: a multifaceted group of syndromes. NeuroRx 2006;3:254-63.
10. Freeze HH. Genetic defects in the human glycome. Nat Rev Genet 2006;7:537-51.
11. Matthijs G, Schollen E, Pardon E, Veiga-Da-Cunha M, Jaeken J, Cassiman JJ, et al. Mutations in PMM2, a phosphomannomutase gene on chromosome 16p13, in carbohydrate-deficient glycoprotein type I syndrome (Jaeken syndrome). Nat Genet 1997;16:88-92.
12. Jaeken J. Congenital disorders of glycosylation. Ann N Y Acad Sci 2010;1214:190-8.
13. Kjaergaard S. Congenital disorders of glycosylation type Ia and Ib. Genetic, biochemical and clinical studies. Dan Med Bull 2004;51:350-63.
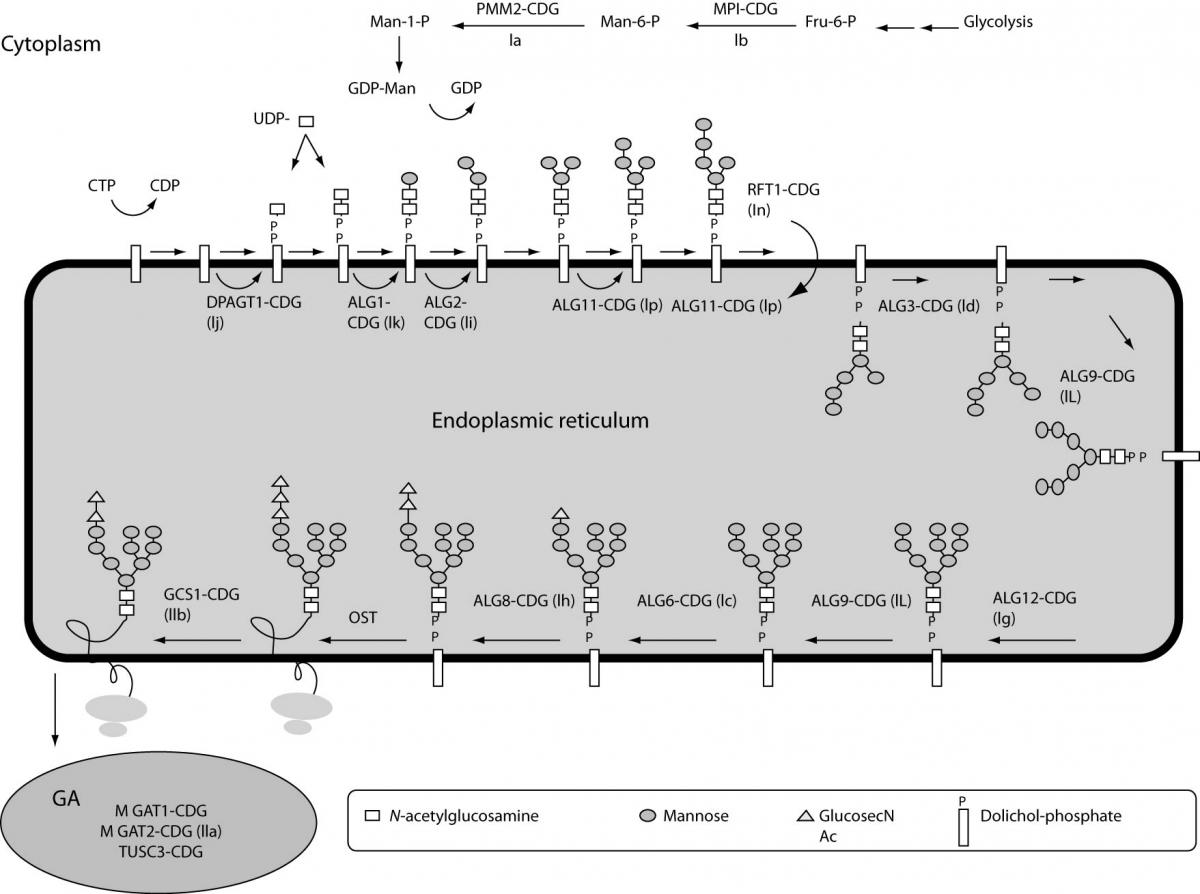
14. Haeuptle MA, Hennet T. Congenital disorders of glycosylation: an update on defects affecting the biosynthesis of dolichol-linked oligosaccharides. Hum Mutat 2009;30:1628-41.
15. Matthijs G, Schollen E, Van Schaftingen E, Cassiman JJ, Jaeken J. Lack of homozygotes for the most frequent disease allele in carbohydrate-deficient glycoprotein syndrome type 1A. Am J Hum Genet 1998;62:542-50.
16. Matthijs G, Schollen E, Bjursell C, Erlandson A, Freeze H, Imtiaz F, et al. Mutations in PMM2 that cause congenital disorders of glycosylation, type Ia (CDG-Ia). Hum Mutat 2000;16:386-94.
17. Kjaergaard S. Congenital disorders of glycosylation type Ia and Ib. Dan Med Bull 2004;51:350-63.
18. Coman D, McGill J, MacDonald R, Morris D, Klingberg S, Jaeken J, et al. Congenital disorder of glycosylation type 1a: three siblings with a mild neurological phenotype. J Clin Neurosci 2007;14:668-72.
19. Jaeken J, Stibler H, Hagberg B. The carbohydrate-deficient glycoprotein syndrome. A new inherited multisystemic disease with severe nervous system involvement. Acta Paediatr Scand Suppl 1991;375:1-71.
20. Jaeken J. Komrower Lecture. Congenital disorders of glycosylation (CDG): it’s all in it! J Inherit Metab Dis 2003;26:99-118.
21. Grunewald S. The clinical spectrum of phosphomannomutase 2 deficiency (CDG-Ia). Biochim Biophys Acta 2009;1792:827-34.
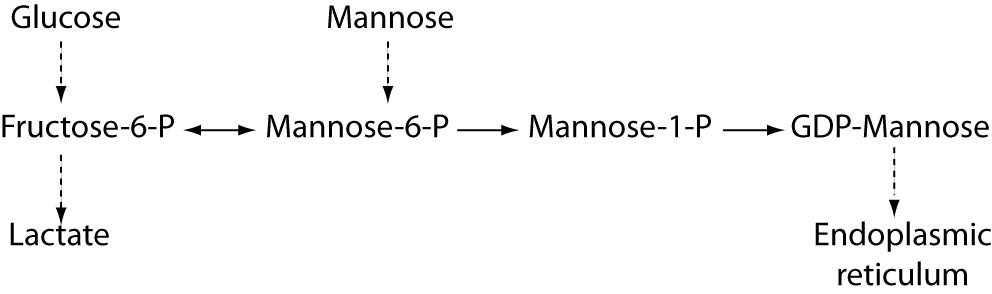
22. Niehues R, Hasilik M, Alton G, Korner C, Schiebe-Sukumar M, Koch HG, et al. Carbohydrate-deficient glycoprotein syndrome type Ib. Phosphomannose isomerase deficiency and mannose therapy. J Clin Invest 1998;101:1414-20.
23. Grunewald S, Imbach T, Huijben K, Rubio-Gozalbo ME, Verrips A, de Klerk JB, et al. Clinical and biochemical characteristics of congenital disorder of glycosylation type Ic, the first recognized endoplasmic reticulum defect in N-glycan synthesis. Ann Neurol 2000;47:776-81.
24. Marquardt T, Denecke J. Congenital disorders of glycosylation: review of their molecular bases, clinical presentations and specific therapies. Eur J Pediatr 2003;162:359-79.
25. Damen G, de Klerk H, Huijmans J, den Hollander J, Sinaasappel M. Gastrointestinal and other clinical manifestations in 17 children with congenital disorders of glycosylation type Ia, Ib, and Ic. J Pediatr Gastroenterol Nutr 2004;38:282-7.
26. Sun L, Eklund EA, Van Hove JL, Freeze HH, Thomas JA. Clinical and molecular characterization of the first adult congenital disorder of glycosylation (CDG) type Ic patient. Am J Med Genet A 2005;137:22-6.
27. Newell JW, Seo NS, Enns GM, McCraken M, Mantovani JF, Freeze HH. Congenital disorder of glycosylation Ic in patients of Indian origin. Mol Genet Metab 2003;79:221-8.
28. Burda P, Borsig L, de Rijk-van Andel J, Wevers R, Jaeken J, Carchon H, et al. A novel carbohydrate-deficient glycoprotein syndrome characterized by a deficiency in glucosylation of the dolichol-linked oligosaccharide. J Clin Invest 1998;102:647-52.
29. Imbach T, Burda P, Kuhnert P, Wevers RA, Aebi M, Berger EG, et al. A mutation in the human ortholog of the Saccharomyces cerevisiae ALG6 gene causes carbohydrate-deficient glycoprotein syndrome type-Ic. Proc Natl Acad Sci U S A 1999;96:6982-7.
30. Al-Owain M, Mohamed S, Kaya N, Zagal A, Matthijs G, Jaeken J. A novel mutation and first report of dilated cardiomyopathy in ALG6-CDG (CDG-Ic): a case report. Orphanet J Rare Dis 2010;5:7.
31. Westphal V, Xiao M, Kwok PY, Freeze HH. Identification of a frequent variant in ALG6, the cause of Congenital Disorder of Glycosylation-Ic. Hum Mutat 2003;22:420-1.
32. Vuillaumier-Barrot S, Le Bizec C, Durand G, Seta N. The T911C (F304S) substitution in the human ALG6 gene is a common polymorphism and not a causal mutation of CDG-Ic. J Hum Genet 2001;46:547-8.
33. Westphal V, Kjaergaard S, Schollen E, Martens K, Grunewald S, Schwartz M, et al. A frequent mild mutation in ALG6 may exacerbate the clinical severity of patients with congenital disorder of glycosylation Ia (CDG-Ia) caused by phosphomannomutase deficiency. Hum Mol Genet 2002;11:599-604.
34. Goreta SS, Dabelic S, Pavlinic D, Lauc G, Dumic J. Frequency Determination of alpha-1,3 Glucosyltransferase p.Y131H and p.F304S Polymorphisms in the Croatian Population Revealed Five Novel Single Nucleotide Polymorphisms in the hALG6 Gene. Genet Test Mol Biomarkers 2012;16:50-3.
35. Rimella-Le-Huu A, Henry H, Kern I, Hanquinet S, Roulet-Perez E, Newman CJ, et al. Congenital disorder of glycosylation type Id (CDG Id): phenotypic, biochemical and molecular characterization of a new patient. J Inherit Metab Dis 2008;31 Suppl2:S381-6.
36. Kranz C, Basinger AA, Gucsavas-Calikoglu M, Sun L, Powell CM, Henderson FW, et al. Expanding spectrum of congenital disorder of glycosylation Ig (CDG-Ig): sibs with a unique skeletal dysplasia, hypogammaglobulinemia, cardiomyopathy, genital malformations, and early lethality. Am J Med Genet A 2007;143A:1371-8.
37. Stolting T, Omran H, Erlekotte A, Denecke J, Reunert J, Marquardt T. Novel ALG8 mutations expand the clinical spectrum of congenital disorder of glycosylation type Ih. Mol Genet Metab 2009;98:305-9.
38. Kranz C, Denecke J, Lehle L, Sohlbach K, Jeske S, Meinhardt F, et al. Congenital disorder of glycosylation type Ik (CDG-Ik): a defect of mannosyltransferase I. Am J Hum Genet 2004;74:545-51.
39. Jaeken J, Vleugels W, Regal L, Corchia C, Goemans N, Haeuptle MA, et al. RFT1-CDG: Deafness as a novel feature of congenital disorders of glycosylation. J Inherit Metab Dis 2009; DOI:10.1007/s10545-009-1297-3.
40. Jennes I, de Jong D, Mees K, Hogendoorn PC, Szuhai K, Wuyts W. Breakpoint characterization of large deletions in EXT1 or EXT2 in 10 multiple osteochondromas families. BMC Med Genet 2011;12:85.
41. Jennes I, Pedrini E, Zuntini M, Mordenti M, Balkassmi S, Asteggiano CG, et al. Multiple osteochondromas: mutation update and description of the multiple osteochondromas mutation database (MOdb). Hum Mutat 2009;30:1620-7.
42. Schmale GA, Conrad EU, 3rd, Raskind WH. The natural history of hereditary multiple exostoses. J Bone Joint Surg Am 1994;76:986-92.
43. Stancheva-Ivanova MK, Wuyts W, van Hul E, Radeva BI, Vazharova RV, Sokolov TP, et al. Clinical and molecular studies of EXT1/EXT2 in Bulgaria. J Inherit Metab Dis 2011;34:917-21.
44. Kranz C, Jungeblut C, Denecke J, Erlekotte A, Sohlbach C, Debus V, et al. A defect in dolichol phosphate biosynthesis causes a new inherited disorder with death in early infancy. Am J Hum Genet 2007;80:433-40.
45. Ungar D, Oka T, Vasile E, Krieger M, Hughson FM. Subunit architecture of the conserved oligomeric Golgi complex. J Biol Chem 2005;280:32729-35.
46. Ungar D, Oka T, Brittle EE, Vasile E, Lupashin VV, Chatterton JE, et al. Characterization of a mammalian Golgi-localized protein complex, COG, that is required for normal Golgi morphology and function. J Cell Biol 2002;157:405-15.
47. Foulquier F. COG defects, birth and rise! Biochim Biophys Acta 2009;1792:896-902.
48. Ng BG, Sharma V, Sun L, Loh E, Hong W, Tay SK, et al. Identification of the first COG-CDG patient of Indian origin. Mol Genet Metab 2011;102:364-7.
49. Mohamed M, Kouwenberg D, Gardeitchik T, Kornak U, Wevers RA, Morava E. Metabolic cutis laxa syndromes. J Inherit Metab Dis 2011;34:907-16.
50. Morava E, Lefeber DJ, Urban Z, de Meirleir L, Meinecke P, Gillessen Kaesbach G, et al. Defining the phenotype in an autosomal recessive cutis laxa syndrome with a combined congenital defect of glycosylation. Eur J Hum Genet 2008;16:28-35.
51. Kornak U, Reynders E, Dimopoulou A, van Reeuwijk J, Fischer B, Rajab A, et al. Impaired glycosylation and cutis laxa caused by mutations in the vesicular H+-ATPase subunit ATP6V0A2. Nat Genet 2008;40:32-4.
52. Wild MK, Luhn K, Marquardt T, Vestweber D. Leukocyte adhesion deficiency II: therapy and genetic defect. Cells Tissues Organs 2002;172:161-73.
53. Peters V, Penzien JM, Reiter G, Korner C, Hackler R, Assmann B, et al. Congenital disorder of glycosylation IId (CDG-IId) - a new entity: clinical presentation with Dandy-Walker malformation and myopathy. Neuropediatrics 2002;33:27-32.
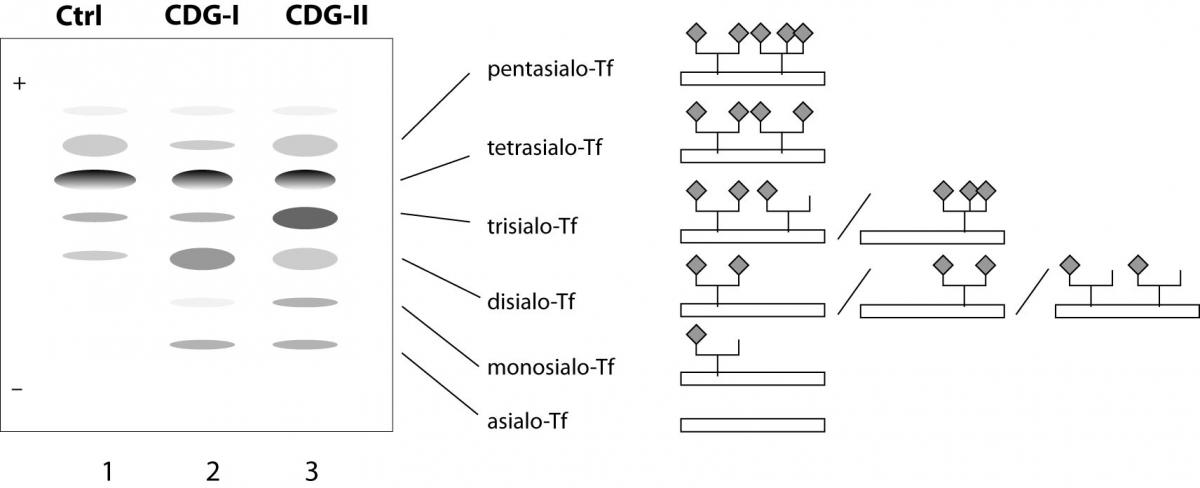
54. Sturiale L, Barone R, Garozzo D. The impact of mass spectrometry in the diagnosis of congenital disorders of glycosylation. J Inherit Metab Dis 2011;34:891-9.
55. Fujita M, Satoh C, Asakawa J, Nagahata Y, Tanaka Y, Hazama R, et al. Electrophoretic variants of blood proteins in Japanese. VI. Transferrin. Jinrui Idengaku Zasshi 1985;30:191-200.
56. Kamboh MI, Ferrell RE. Human transferrin polymorphism. Hum Hered 1987;37:65-81.
57. Helander A, Eriksson G, Stibler H, Jeppsson JO. Interference of transferrin isoform types with carbohydrate-deficient transferrin quantification in the identification of alcohol abuse. Clin Chem 2001;47:1225-33.
58. Carchon HA, Chevigne R, Falmagne JB, Jaeken J. Diagnosis of congenital disorders of glycosylation by capillary zone electrophoresis of serum transferrin. Clin Chem 2004;50:101-11.
59. Quintana E, Montero R, Casado M, Navarro-Sastre A, Vilaseca MA, Briones P, et al. Comparison between high performance liquid chromatography and capillary zone electrophoresis for the diagnosis of congenital disorders of glycosylation. J Chromatogr B Analyt Technol Biomed Life Sci 2009;877:2513-8.
60. Barone R, Sturiale L, Garozzo D. Mass spectrometry in the characterization of human genetic N-glycosylation defects. Mass Spectrom Rev 2009;28:517-42.
61. Wada Y, Nishikawa A, Okamoto N, Inui K, Tsukamoto H, Okada S, et al. Structure of serum transferrin in carbohydrate-deficient glycoprotein syndrome. Biochem Biophys Res Commun 1992;189:832-6.
62. Lacey JM, Bergen HR, Magera MJ, Naylor S, O’Brien JF. Rapid determination of transferrin isoforms by immunoaffinity liquid chromatography and electrospray mass spectrometry. Clin Chem 2001;47:513-8.
63. Sturiale L, Barone R, Palmigiano A, Ndosimao CN, Briones P, Adamowicz M, et al. Multiplexed glycoproteomic analysis of glycosylation disorders by sequential yolk immunoglobulins immunoseparation and MALDI-TOF MS. Proteomics 2008;8:3822-32.
64. Guillard M, Morava E, van Delft FL, Hague R, Korner C, Adamowicz M, et al. Plasma N-glycan profiling by mass spectrometry for congenital disorders of glycosylation type II. Clin Chem 2011;57:593-602.
65. Faid V, Chirat F, Seta N, Foulquier F, Morelle W. A rapid mass spectrometric strategy for the characterization of N- and O-glycan chains in the diagnosis of defects in glycan biosynthesis. Proteomics 2007;7:1800-13.
66. Mills K, Mills P, Jackson M, Worthington V, Beesley C, Mann A, et al. Diagnosis of congenital disorders of glycosylation type-I using protein chip technology. Proteomics 2006;6:2295-304.
67. Schwarz M, Thiel C, Lubbehusen J, Dorland B, de Koning T, von Figura K, et al. Deficiency of GDP-Man:GlcNAc2-PP-dolichol mannosyltransferase causes congenital disorder of glycosylation type Ik. Am J Hum Genet 2004;74:472-81.
68. Simpson MA, Cross H, Proukakis C, Priestman DA, Neville DC, Reinkensmeier G, et al. Infantile-onset symptomatic epilepsy syndrome caused by a homozygous loss-of-function mutation of GM3 synthase. Nat Genet 2004;36:1225-9.
69. Jaeken J. Congenital disorders of glycosylation (CDG): update and new developments. J Inherit Metab Dis 2004;27:423-6.
70. Krawitz PM, Schweiger MR, Rodelsperger C, Marcelis C, Kolsch U, Meisel C, et al. Identity-by-descent filtering of exome sequence data identifies PIGV mutations in hyperphosphatasia mental retardation syndrome. Nat Genet 2010;42:827-9.
71. Goreta SS, Dabelic S, Dumic J. Employment of single-strand conformation polymorphism analysis in screening for alpha-1,3 glucosyltransferase gene mutation A333V in Croatian population. J Clin Lab Anal 2011;25:65-70.
72. Bjursell C, Erlandson A, Nordling M, Nilsson S, Wahlstrom J, Stibler H, et al. PMM2 mutation spectrum, including 10 novel mutations, in a large CDG type 1A family material with a focus on Scandinavian families. Hum Mutat 2000;16:395-400.
73. Imbach T, Grunewald S, Schenk B, Burda P, Schollen E, Wevers RA, et al. Multi-allelic origin of congenital disorder of glycosylation (CDG)-Ic. Hum Genet 2000;106:538-45.
74. Mizugishi K, Yamanaka K, Kuwajima K, Yuasa I, Shigemoto K, Kondo I. Missense mutations in the phosphomannomutase 2 gene of two Japanese siblings with carbohydrate-deficient glycoprotein syndrome type I. Brain Dev 1999;21:223-8.
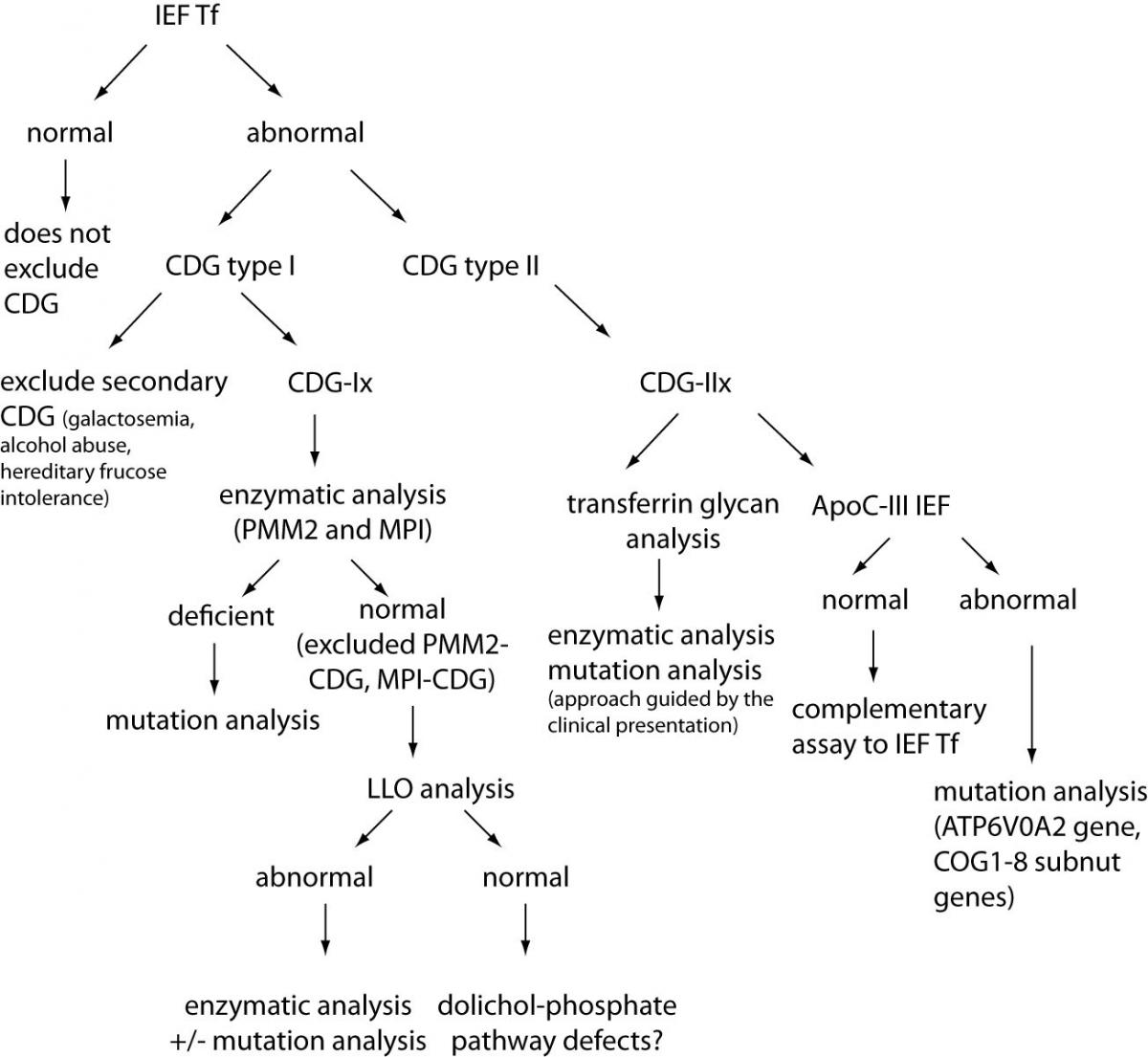
75. Lefeber DJ, Morava E, Jaeken J. How to find and diagnose a CDG due to defective N-glycosylation. J Inherit Metab Dis 2011;34:849-52.
76. Jones MA, Bhide S, Chin E, Ng BG, Rhodenizer D, Zhang VW, et al. Targeted polymerase chain reaction-based enrichment and next generation sequencing for diagnostic testing of congenital disorders of glycosylation. Genet Med 2011;13:921-32.
77. Matthijs G, Schollen E, Van Schaftingen E. The prenatal diagnosis of congenital disorders of glycosylation (CDG). Prenat Diagn 2004;24:114-6.
78. Clayton P, Winchester B, Di Tomaso E, Young E, Keir G, Rodeck C. Carbohydrate-deficient glycoprotein syndrome: normal glycosylation in the fetus. Lancet 1993;341:956.
79. Nogueira C, Quelhas D, Vilarinho L. Prenatal diagnosis for CDG Ia based on post-mortem molecular study of Guthrie card. Mol Genet Metab 2006;87:379.
80. Charlwood J, Clayton P, Keir G, Mian N, Young E, Winchester B. Prenatal diagnosis of the carbohydrate-deficient glycoprotein syndrome type 1A (CDG1A) by a combination of enzymology and genetic linkage analysis after amniocentesis or chorionic villus sampling. Prenat Diagn 1998;18:693-9.
81. Thiel C, Korner C. Mouse models for congenital disorders of glycosylation. J Inherit Metab Dis 2011;34:879-89.
82. Schneider A, Thiel C, Rindermann J, Derossi C, Popovici D, Hoffmann GF, et al. Successful prenatal mannose treatment for congenital disorder of glycosylation-Ia in mice. Nat Med 2011;18:71-3.
83. Panneerselvam K, Freeze HH. Mannose corrects altered N-glycosylation in carbohydrate-deficient glycoprotein syndrome fibroblasts. J Clin Invest 1996;97:1478-87.
84. Schroeder AS, Kappler M, Bonfert M, Borggraefe I, Schoen C, Reiter K. Seizures and stupor during intravenous mannose therapy in a patient with CDG syndrome type 1b (MPI-CDG). J Inherit Metab Dis 2011;DOI:10.1007/s10545-010-9252-x.
85. Marquardt T, Luhn K, Srikrishna G, Freeze HH, Harms E, Vestweber D. Correction of leukocyte adhesion deficiency type II with oral fucose. Blood 1999;94:3976-85.
86. Georgiou E, Layton M, Karadimitris A. Inherited GPI deficiency: a disorder of histone hypoacetylation. Birth Defects Res C Embryo Today 2009;87:327-34.
87. Almeida AM, Murakami Y, Baker A, Maeda Y, Roberts IA, Kinoshita T, et al. Targeted therapy for inherited GPI deficiency. N Engl J Med 2007;356:1641-7.
88. Eklund EA, Merbouh N, Ichikawa M, Nishikawa A, Clima JM, Dorman JA, et al. Hydrophobic Man-1-P derivatives correct abnormal glycosylation in Type I congenital disorder of glycosylation fibroblasts. Glycobiology 2005;15:1084-93.
89. Haeuptle MA, Welti M, Troxler H, Hulsmeier AJ, Imbach T, Hennet T. Improvement of dolichol-linked oligosaccharide biosynthesis by the squalene synthase inhibitor zaragozic acid. J Biol Chem 2011;286:6085-91.
90. Sharma V, Ichikawa M, He P, Bravo Y, Dahl R, Ng BG, et al. Phosphomannose Isomerase Inhibitors Improve N-Glycosylation in Selected Phosphomannomutase-deficient Fibroblasts. J Biol Chem 2011;286:39431-8.