References
1. Büttner J. [Statistische Qualitätskontrolle in der Klinischen Chemie]. Z Klin Chem 1967;5:41-8. (in German)
2. [Richtlinien der Bundesärztekammer zur Durchführung von Maßnahmen der statistischen Qualitätskontrolle und von Ringversuchen im Bereich der Heilkunde]. Dtsch Ärztebl 1971;68:2228-31. (in German)
3. Keller H, Guder WG, Hansert E, Stamm D. Biological influence factors and interference factors in clinical chemistry: general considerations. Clin Chem Clin Biochem 1985;23:3-6.
4. Richterich R. [Klinische Chemie]. Theorie und Praxis. Basel: S Karger; 1964. (in German)
5. Bonini PA, Plebani M, Ceriotti F, Rubboli F. Errors in laboratory medicine. Clin Chem 2002;48:691-8.
6. Statland BE, Winkel P. Effects of preanalytical factors on the intraindividual variation of analytes in the blood of healthy subjects: consideration of preparation of the subject and time of venipuncture. Crit Rev Clin Lab Sci 1977;8:105-44.
http://dx.doi.org/10.3109/10408367709151694.
7. Guder WG. [Einflussgrößen und Störfaktoren bei klinisch chemischen Untersuchungen]. Internist 1980;21:533-42. (in German)
8. Guder WG. [Einfluss von Probennahme, Probentransport und Probenverwahrung auf klinisch chemische Untersuchungsergebnisse]. Ärztl Lab 1976;22:69-75. (in German)
9. Tryding N, Tufvesson C, Sonntag O. Drug Effects in Clinical Chemistry. Analytical Interferences and Biological Effects of Drugs on Biochemical and Haematological Laboratory Investigations. 7th ed. Stockholm: AB Realtyck; 1996.
10. Young D. Effects of Drugs on Clinical Laboratory Tests, Washington: AACC Press; 1990.
11. Sonntag O. Haemolysis as an interference factor in clinical chemistry. J Clin Chem Clin Biochem 1986;24:127-39.
12. Guder WG, da Fonseca-Wollheim F, Heil W, Schmitt YM, Töpfer G, Wisser H, Zawta B. The haemolytic, icteric and lipemic sample. Recommendations regarding their recognition and prevention of clinically relevant interferences. J Lab Med 2000;24:357-64.
13. Peters JP, Van Slyke DD. Quantitative Clinical Chemistry. Interpretations Vol 1. Baltimore: Williams and Wilkins; 1946.
14. Einer G, Zawta B. [Präanalytikfibel. Kooperation von Arzt und Labor]. Leipzig: Johann Ambrosius Barth; 1987. (in German)
15. Young DS. Effects of preanalytical variables on clinical laboratory tests. Wasshington: AACC Press; 1993.
16. Guder WG, Narayanan S, Wisser H, Zawta B. Samples: From the Patient to the Laboratory. The Impact of Preanalytical Variables on the Quality of Laboratory Results. Darmstadt: GIT-Verlag; 1996 (4th ed. Diagnostic Samples: From the Patient to the Laboratory. Weinheim: Wiley-Blackwell; 2009).
17. Guder WG, Hagemann P, Wisser H, Zawta B. [Fokus Patientenprobe; Kompendium Präanalytik]. CD-Rom; Heidelberg: Schwechat, Basel BD; 2007. (in German)
18. Dybkaer R. Vocabulary for use in measurement procedures and description of reference material in laboratory medicine. Eur J Clin Chem Clin Biochem 1997:40:1416-20.
19. Clinical Laboratory Standards Institute (CLSI), Collection, Transport and processing of blood specimen for testing plasma-based coagulation assays. CLSI, Document H4-A5. Approved standard 6th ed. Clinical Laboratory Standards Institute, Wayne, Pennsylvania, USA, 2004.
20. International Organization for Standardization, European Commiteee for Standardization, Deutsches Institut für Normung (ISO/EN/DIN 15189). Medical Laboratories - Particular Requirements for Quality and Competence. Geneva: ISO; 2007.
21. Guder WG, Wahlefeld AW. Specimens and samples in clinical laboratory; the preanalytical phase. In: Bergmeyer HU. Methods of Enzymatic Analysis. 3. Ed. Weinheim: Verlag Chemie Vol II; 1983. pp. 2-20.
22. Wisser H. [Präanalytik in Greiling, Gressner Lehrbuch der Klinischen Chemie und Pathobiochemie]. Stuttgart, New York: Schattauer; 1987. pp.37-49. (in German)
23. Hagemann P. Preanalytical Phase, in Thomas L. Laboratory and Diagnosis. Frankfurt: TH-Books; 2005. pp.1965-74.
24. Ricos C, Alvarez V, Cava F, Garcia-Lario JV, Hernandez A, Jiminez CV, et al. Current databases on biological variation: pros et cons and progress. Scand J Clin Lab Invest 1999;59:491-500.
http://dx.doi.org/10.1080/00365519950185229.
25. Ricos C, Biosca C, Ibarz M, Minchinela J, Llopis M, Perich C, et al. Quality indicators and specifications for strategic and support processes in laboratory medicine. Clin Chem Lab Med 2008;46:1189-94.
http://dx.doi.org/10.1515/CCLM.2008.225.
26. The Impact of the Preanalytical Phase on the Quality of Laboratory Results. 1. European Meeting on the Pre-Analytical Phase in Laboratory Sciences. Proceedings. Tampere, Finland, July 1-2, 1995. Meylan: Becton Dickinson Vacutainer Systems and Labware; 1995.
27. The Impact of the Pre-Analytical Phase on the Quality of Laboratory Results in Haemostasis. Proceedings. 1st Symposium. Montpellier, France, October 14, 1996. Meylan: Becton-Dickinson Vacutainer Systems; 1996.
28. The Impact of the Pre-Analytical Phase on the Quality of Laboratory Results. Proceedings. 2. Symposium. Oxford, July 5-7, 1996. Meylan: Becton-Dickinson Vacutainer Systems; 1996.
29. The Impact of the Preanalytical Phase on the Quality of Laboratory Results. Proceedings, 3rd Symposium; European expert meeting; FESCC Educational Program. Basel August 15-16, 1997. Meylan: Becton-Dickinson Vacutainer Systems; 1997.
30. Biological and Technical Aspects of the Preanalytical Phase in Clinical Chemistry and Laboratory Medicine. Fourth expert symposium. Proceedings. Karlovy Vary, September 24-25, 1998. Meylan: Becton-Dickinson Vacutainer Systems Europe; 1998.
31. Quality of the Preanalytical Phase in Europe. Satellite meeting of the Euromedlab. Prague, Czech Republic, May 26, 2001. Leuwen: Terumo Europe; 2001.
32. Pre-Analytical Phase on the Quality of Laboratory Results, a satellite symposium of the IFCC 2002, Kyoto; Tokyo. Leuwen: Terumo Corp Europe; 2002.
33. World Health Organization. Use of Anticoagulants in Diagnostic Laboratory Investigations and Stability of blood plasma and serum samples. 2002 Geneva, WHO and WHO/DIL/LAB/99.1 Rev.2.
34. Guder WG, Ehret W, da Fonseca-Wollheim F, Heil W, Müller Plathe O, Töpfer G, et al. [Die Qualität diagnostischer Proben]. 1. Auflage Deutsche Gesellschaft für Clinische Chemie und Deutsche Gesellschaft für Laboratoriumsmedizin, 1999; Heidelberg Becton Dickinson GmbH. (in German)
35. Lippi G, Becan-McBride K, Behulova D, Bowen RA, Church S, Delange J, et al. Preanalytical quality improvement: in quality we trust. Clin Chem Lab Med 2013:51:229-41.
36. European Federation of Clinical Chemistry and Laboratory Medicine (EFLM). 2nd EFLM-BD European conference on preanalytical phase. Preanalytical quality improvement - in quality we trust. Biochem Med 2013:23:A1-55.
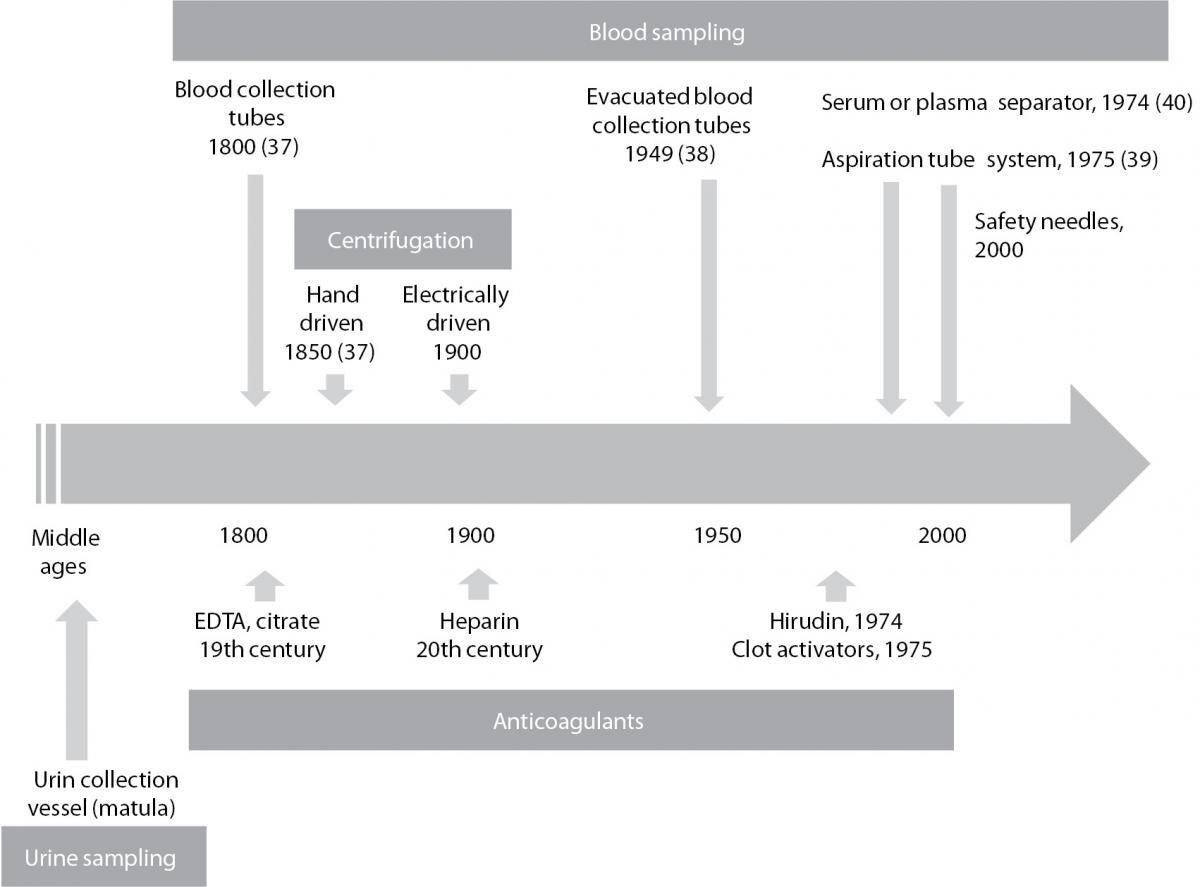
37. Senses, Sensors and Systems. A journey through the history of laboratory diagnosis. Editiones Roche 2004.
39. Sarstedt international. 50 years of Sarstedt 1961-2011. Nümbrecht Sarstedt AG; 2011.
40. Coleman CM. Separation float for blood collection tubes with water swellable material. April 7, 1998; US Patent 5,736,033.
41. Price CP, Christenson RH. Evidence based Laboratory Medicine. Washington: AACC Press; 2003.
42. Hofmann W, Ehrich JHH, Guder WG, Keller F, Scherberich J. Diagnostic pathways for exclusion and diagnosis of kidney diseases. Clin Lab 2012;58:871-89.